Instagram Live with Dr. Levita D’Souza
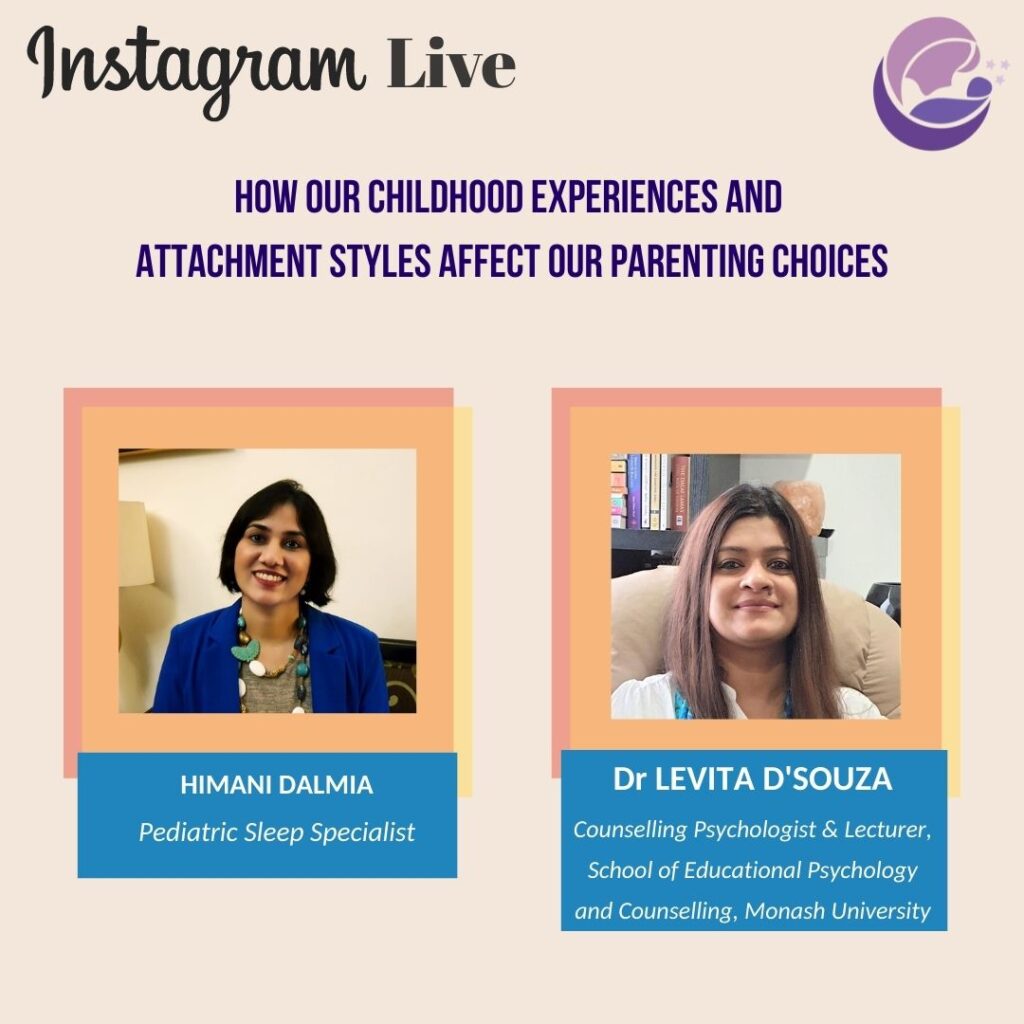
Instagram Live with Dr. Levita D’souza I had a riveting conversation with Counselling Psychologist and Researcher, Dr Levita D’Souza, on Instagram Live, where we talked about attachment theory, attachment styles, how our own childhood experiences affect our parenting choices, ruptures and repairs in the bonding process with our babies and children, how parentj g is an opportunity for personal growth and much more! Unfortunately, there were some disturbances in the audio. So that Levita’s amazing insights don’t get lost, I am sharing a transcript for the conversation here. Do read through until the very end so that you don’t miss some transformative truth bombs! How our childhood experiences and attachment styles affect our parenting choices. Himani: Hi everyone. Thank you for joining in for this live with Levita D’Souza. I’m super excited because every conversation I have with Levita is just full of these truth bombs that she tends to drop. Levita is a Registered Counseling Psychologist and Lecturer within the Faculty of Education at Monash University in Melbourne, Australia. Her research interests are in the area of perinatal psychology, adverse childhood experiences and its impact on attachment patterns and subsequent parenting practices. Within this space, her current research projects are looking at psychological factors affecting first-time fathers as they transition to fatherhood and father-child bonding. She’s also undertaking research on cultural influences on parenting choices in relation to infant sleep. So that’s really where Levita and I have had many conversations – where infant sleep is concerned. And, as an Indian living in a sort of industrialized, westernized – “westernized”, not “Western” – country, I’m sure you’ve faced this dichotomy and perhaps that was one of the factors that drew you towards this research. So, could you tell us a little bit about your journey and what drew you to your current work? Levita: Yes, I think my journey first started with my quest and questioning around mental illness. Why people are mentally ill; if it runs in families, does it mean I’m doomed; does it mean that we cannot do things differently. And that led to my early work in my early study working with families where there has been mental illness. And what I found was that some outcomes were much better than others. So, for some patients, the outcomes were much better than others. And the same sort of thing was replicated when I was working with children who had experienced trauma. You know, crap happens to everyone. But some children were better able to deal with the trauma and overcome it or manage their symptoms compared to others. And what I could see clearly was those early sorts of parenting experiences. And it wasn’t till I became a mum myself and I started to question why – who am I as a mother? What kind of a mother do I want to be? What from my own parenting experiences do I want to bring into how I parent my child? What do I not want? – that I started to really dabble in this thing of attachment theory and how that can influence – those really early experiences can influence – later outcomes for children. And so then I’ve landed in this space where, very crudely, I say “how not to be a jerk of a parent”. That’s what the transition to parenthood is. What influences us, what will help us be better parents? What do we draw on? What do we not draw on? What do we want to leave behind? And attachment, I think plays a big role in that. Himani: So, you know, just for some of us and the uninitiated and the layperson, the lay parent rather, could you very simply explain attachment theory – what you spend years teaching your students – in about two minutes? (laughter) Levita: I’ll try. I will try. I was reflecting on this and going, “can I reliably do it?” But I’m going to try this. So, very simply… Himani: You can take ten minutes. I’m joking about the two minutes. Levita: Thank you! Much appreciated (laughter). So, very simply, it’s like a bond. It’s a bond that exists between the baby and the caregiver. For the purpose of this talk, I will interchange between “caregiver” and “mother” but I want to absolutely acknowledge that families come in all forms and so it can be the father, it can be the grandmother, or any caregiver who is consistent, who is reliable, who is dependable, who is sensitive, and who is able to attune to the baby in a timely sort of way. And so, what is attachment? It’s a bond between the baby and the caregiver. Why does it exist? It exists purely and solely for the purpose of survival. So, when the baby is born, the baby is born with a system, what we call a “bio-behavioural system”, which it uses to cue the parent that they need things, to meet their needs. So, let’s take an example, here’s a little baby. They experience hunger, and they experience hunger on a very physiological level, right, it’s a biological behaviour. That hunger puts the baby’s system in chaos. It experiences pain. The baby doesn’t immediately cry. What the baby might do earlier to cue the parent would be root, stick their tongue out, put their hand to their mouth, and these are, sort of, very early signs where the baby is cuing in the caregiver to say, “Mamma, look at me, I have a need, I’m expressing this, attune to me, meet my need, make me feel good.” When the baby does that, the mother goes, “oh, you’re hungry! You want me to pick you up, let me feed you.” When the mother meets that need, the baby’s system – that had started to be in chaos because of the hunger – returns to this really calm, nice, happy place. Mum feels good because baby has stopped crying; baby feels good because baby’s needs
Should I follow the EASY routine?

Should I follow the EASY routine? No! Please follow the exact opposite. The “Eat – Activity – Sleep – You” routine is a pet concept of sleep trainers. It is heavily marketed as a quick-fix mantra for baby sleep but is, in fact, such a bizarre concept that it is really no wonder that millions of flummoxed parents try to follow it but find themselves either failing miserably or entering a never-ending cycle of training and disconnected parenting. The EASY routine is based on the idea that babies should eat (nurse/bottle feed), then play or engage in some activity and then sleep. Basically, they should not “feed to sleep”. The logic being that a baby who feeds to sleep will develop a “bad sleep association” and will need feeding after every sleep cycle to sleep again. This is totally senseless for so many reasons, starting with: 1. Babies are biologically programmed to feed to sleep. The suckling motion promotes sleep. Breastmilk contains sleepy hormones that help baby sleep. In fact, feeding to sleep is nature’s perfectly designed solution to baby sleep. 2. Babies may in fact even get hungry while they sleep. 3. Babies WANT to feed to sleep and will inevitably cry or resist sleep if denied the breast or bottle. This will lead to a cycle of sleep training. 4. Babies do wake at the end of sleep cycles and feeding is one of the easiest ways to help them enter the next sleep cycle. The idea that they will “self-soothe” if they do not have a sleep association is unscientific as babies are incapable of self-soothing. Oh, and please do not miss the YOU at the end. Apparently, once the baby is asleep, it’s free time for YOU. And somehow, I doubt sleep trainers mean enjoying an audiobook while holding your sleeping baby or taking a nap for yourself next to said baby! Nothing as comforting to the baby as that.
Why can’t I just let my baby sleep when tired? Why all this drama?

Why can’t I just let my baby sleep when tired? Why all this drama? Because it won’t happen. In the beginning, we all try this. Very few of us go into parenting believing anything other than “baby will just fall asleep when tired”. However, we learn fairly quickly that this is not the case. Why is this: 1. Babies are unable to soothe themselves to sleep. If they fall asleep on their own, it is when they are tired to the point of exhaustion. 2. Overtired babies sleep badly because their bodies fill with the stress hormone cortisol. 3. Our modern environments are not conducive to baby sleep. 4. Babies who fell asleep whenever, wherever in pre-modern times were usually wrapped to their parents all day, nursing and sleeping on demand. 5. Artificial light for the last century has wreaked havoc with circadian rhythms. 6. Babies that our “elders” tell us about were likely grossly overtired or were sleeping in cloth cradles or…our elders don’t really remember. 7. “Other people’s babies” who fall asleep everywhere and anywhere are either grossly overtired or sleep trained (knowingly or unknowingly). If we attempt to make our babies fall asleep of their own accord, we are likely to end up with cranky, overtired babies who take short naps, cry before and after naps, seem fussy through the day, don’t eat well, wake more frequently at night, cry at night, have active nightwakings and wake early in the mornings. If that isn’t reason enough to practice a little sleep management and give our babies the support they need, I don’t know what is!🙂
My most prized baby related possession

My most prized baby related possession What do you think is my most prized baby related investment? The cot? Nope. It’s a repository of stuffed animals. The stroller? Delhi isn’t really a walking city, sadly. The breastpump? Too cumbersome and it was honestly easier to just lug baby everywhere with me. Expensive toys? They were played with twice each. The baby carrier? Ok, that comes pretty close. But, honestly, my most prized possession is the video baby monitor. It is my lifeline. With my video monitor, I can watch my babies while they sleep and spot the tiniest stir. I can leave my babies in a pitch dark and quiet room and yet dash back inside as soon as I need to bridge sleep or soothe or comfort. I don’t need to leave a door open and allow light or sound to leak in. I don’t need to wait for my babies to wake up to the extent that they cry or call out. And I don’t need to stay inside with them throughout if I don’t want to. The video baby monitor allows me to step out after bedtime (and once my babies are in deep sleep, often after a long cluster dreamfeeding spell), eat my dinner, finish work, watch TV, spend time with my husband, have some me time without compromising or risking my babies’ sleep in the slightest. I can pop back in to nurse or soothe them as needed and then pop back out again. Once my babies no longer needed to be held for naps, the video monitor became my best friend during the day as well. If you don’t have one already, please don’t even think twice. The video baby monitor will change your life.
Baby sleeping but you can’t? Practice sleep hygiene for yourself too.

Baby sleeping but you can’t? Practice sleep hygiene for yourself too. Baby is sleeping but you are just tossing and turning. Baby has woken up for the nth time at night and gone back to sleep but you are unable to go back to sleep. Baby is finally sleeping through the night after 3.5 years but you are still waking multiple times every night. Sounds familiar? When sleep deprivation becomes a part of our new normal, it becomes important to pay attention to sleep hygiene and healthy sleep practices for ourselves as well, like: 1. Set your body clock – go to sleep and wake up at the same time everyday. 2. Organize your day with a to-do list. Keep a pad and pen next to your bed to jot down any tasks that pop up in your head so that they don’t keep bouncing around in there! 3. Avoid caffeine late in the day – it stays in your bloodstream between 6 and 14 hours! 4. Quit smoking 5. Ask your doctor about side effects of any medication you may be taking 6. Watch out for the effects of too much alcohol – it may cause you to fall asleep but then wake a few hours later and be unable to sleep again 7. Make exercise a part of your day – but more than 3 hours before bedtime 8. Make your environment sleep-friendly – a comfortable bed, the right temperature, no noise, keep it dark. 9. Don’t spend too much awake time in bed as it’s best to associate the bed with sleep. 10. Have your own bedtime routine 11. Eat right and eat light before sleep 12. No screens for at least an hour before bedtime 13. Use progressive relaxation or meditation to slow down your body and mind (you could explore an audio file or app) Wishing you many nights of restful sleep!
Will feeding infant formula help my baby sleep?

Will feeding infant formula help my baby sleep? Although urban legend claims formula fed babies sleep longer, there is no scientific evidence to support this. The few studies that have been done to compare the sleep of breastfed and formula fed babies do not show a statistically significant difference. Anecdotal evidence from parents around us also gives varying reports. Many formula feeding parents are equally sleep deprived and exhausted. Some do testify to longer stretches of sleep. However, there are several other parenting practices that are not accounted in these cases and so it is difficult to draw any solid conclusions. Formula is heavier than breastmilk and takes longer to digest. While this can lead to some longer stretches of sleep in the newborn stage when baby tummies are really very small, the heaviness of formula can also cause stomach troubles like gas which can disturb sleep. Furthermore, the link between a full stomach and long hours of sleep is not strong. If it was, the introduction of solids would ensure breastfed babies too slept longer hours, which doesn’t happen. In fact, breastmilk contains the sleep hormone melatonin, which induces sleep. Breastfed babies wake more easily from active sleep, perhaps due to the sleep hormones. And while this makes them more prone to nightwakings, it is also probably what contributes to the lower risk of SIDS recorded amongst breastfed babies. Studies show that, while breastfed babies may be waking more, breastfeeding mums report more sleep. Nursing mothers benefit from high levels of sleep-inducing hormones like prolactin, experience more than double the normal duration of nocturnal slow wave sleep, and may be able to sleep during night-time feeds, if they bedshare and nurse lying down. Babies sleep longer hours/ sleep through the night when they are developmentally ready for it. They wake for several reasons at night – at the end of sleep cycles or due to some internal or external factor that they are incapable of regulating on their own. No single factor, like milk source, can override this developmental trajectory.
Decoding 3 pieces of sleep jargon

Decoding 3 pieces of sleep jargon: “active nightwakings”, “overtiredness” and “circadian rhythms” Active nightwakings: What we call “active nightwakings” (or “split nights”) are basically occasions when a baby wakes up at night and is not easily soothed back to sleep and wants to wake fully and play. These are different from the normal wakings that are a few seconds or minutes long, where a baby is easily soothed back to sleep through feeding or rocking or, when they are older, with a cuddle. Active nightwakings can be excruciatingly exhausting for parents and, on most occasions, do indicate an issue in the baby’s sleep that can be easily rectified. The second type of waking is a normal part of baby sleep. In fact, all human beings wake several times every night as all of us actually sleep in “cycles” where we transition from light sleep to deep sleep to REM sleep and then back to light sleep. We all wake in between each and every cycle but, as adults, we are able to roll over or pull up a blanket or fluff a pillow or snuggle our partner and fall back asleep, not even realizing that we are actually awake. Babies wake in quite the same way between sleep cycles but they are unable to fall back asleep on their own and need the help of a caregiver to drift back into a new sleep cycle. This is absolutely biologically normal. For breastfed babies, the easiest way to “bridge” sleep cycles is to simply nurse them. Otherwise babies can be bottle-fed or rocked or walked or, once they are older toddlers, patted or cuddled. The brief, non-active wakings are nothing to worry about and are part and parcel of baby sleep. They reduce organically n as babies grow older and develop the ability to connect sleep cycles on their own. There is absolutely no need for any kind of “sleep training” or development of “self-soothing” as the very idea is unscientific. It is akin to “training” our 6-month-olds to “walk” by repeatedly not picking them up. It makes no sense at their developmental stage. The best that we can do is have an age appropriate sleep routine throughout the day and ensure baby is not overtired and has a conducive sleep environment. These steps can go a long way in reducing wakings. The other type of waking – an “active nightwaking” – is different and can be much more exhausting for both babies and parents. After the age of 4 months, when a baby’s circadian rhythms have formed and baby has some concept of day and night, a baby will not usually wake to play at night. If she does, it means something is going on. One possibility is that the baby does not have an age appropriate sleep schedule – meaning, the right number and length of naps, optimum gaps between naps or a suitably early bedtime. Another is that the sleep environment is not conducive, like it isn’t pitch dark and quiet or the temperature is not comfortable. This can all be rectified with some effort and management on the parents’ part. The parent will need to learn about what routine is best for the baby’s current age and then help the baby into that routine by being sensitive to baby’s cues. It is also possible that baby is going through a specific phase like a “nap transition” (shifting from a higher number of naps to a lower number of naps per day) or a “sleep regression” (a temporary disturbance in sleep due to immense cognitive and physical development). In this case, not much can be done and we need to ride it out. It will pass in a few days or a couple of weeks. So, how exactly should we tackle an active nightwaking while it’s happening at night? When baby wakes up, continue to keep it dark. You can soothe baby with your voice and shush baby as you try to make her sleep again by feeding or rocking. If baby does not fall back asleep in about 20 minutes, you may need to throw in the towel and let baby play for a certain amount of time before once again soothing the baby back to sleep. Continuing to soothe an awake baby for over an hour can be extremely frustrating, to no avail. The next morning, though, it’s important to analyse what the reason for the active nightwaking could be in order to figure out how to deal with it. Overtiredness: When we stay awake past our optimum awake window, we are overtired. Think about a day when you’ve felt very tired around 10 pm, sat down to finish some work and then hit the sack around midnight, only to find that you’re feeling wired and awake now, tossing and turning, unable to fall asleep. When our bodies feel tired, they release a stress hormone called “cortisol” to wake us up. Babies are very sensitive to cortisol production. They have certain “awake windows” – spans of time that they can be awake at a certain age – before they need to sleep again, or risk cortisol production. These awake windows are determined by our “homeostatic rhythms”, which create sleep pressure and tell us when to fall asleep (something our “circadian rhythms” do as well, though only at night). Overtiredness is actually the bane of baby sleep. It is extremely important to help our babies fall asleep when we observe early sleep cues. If we miss these cues, our babies’ bodies will fill with the stress hormone, cortisol, and they will suddenly seem awake again – a second rush of energy that is called the “second wind” and that misleads us into thinking our babies are not ready to sleep. Soon, our babies and toddlers will become hyperactive and, eventually, cranky. If we wait till our babies are cranky to recognize that they need to sleep, we will find them to be fussy at the breast
