Instagram Live with Dr. Levita D’Souza
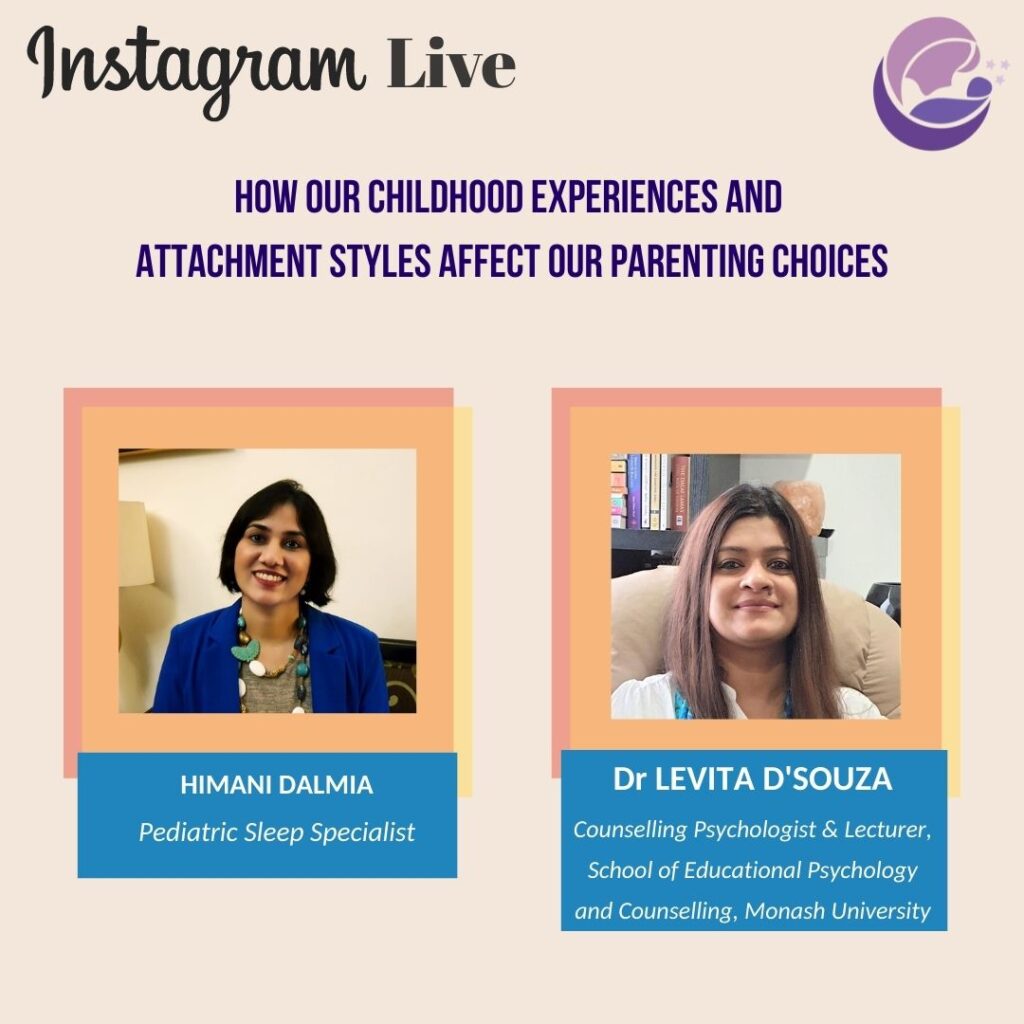
Instagram Live with Dr. Levita D’souza I had a riveting conversation with Counselling Psychologist and Researcher, Dr Levita D’Souza, on
Should I follow the EASY routine?

Should I follow the EASY routine? No! Please follow the exact opposite. The “Eat – Activity – Sleep – You”
Why can’t I just let my baby sleep when tired? Why all this drama?

Why can’t I just let my baby sleep when tired? Why all this drama? Because it won’t happen. In the
My most prized baby related possession

My most prized baby related possession What do you think is my most prized baby related investment? The cot? Nope.
Baby sleeping but you can’t? Practice sleep hygiene for yourself too.

Baby sleeping but you can’t? Practice sleep hygiene for yourself too. Baby is sleeping but you are just tossing and
Will feeding infant formula help my baby sleep?

Will feeding infant formula help my baby sleep? Although urban legend claims formula fed babies sleep longer, there is no
Decoding 3 pieces of sleep jargon

Decoding 3 pieces of sleep jargon: “active nightwakings”, “overtiredness” and “circadian rhythms” Active nightwakings: What we call “active nightwakings” (or
